Caregiving, Health Literacy, Needs Navigation, Trust
In her first post as part of a three-part blog series, Caroline Hoover shares her personal story about why she is passionate about patient advocacy.
NPAF volunteer Caroline Hoover was born and raised in western North Carolina and now attends the University of North Carolina at Chapel Hill. She hopes to practice health care law in order to advance access to care and supports in under-resourced communities. She will be contributing an ongoing blog series about the challenges of accessing health care in Appalachia.
I grew up in rural Appalachia in a history-rich community interwoven with respect, family and a hankering for justice. Etched in the faces of my relatives, neighbors and peers, I witnessed the struggle of poverty, hunger, opioid addiction and the effects of an inaccessible health care system. I was not just an observer of these deeply personal experiences. I, too, experienced a great deal of challenges that exemplified the strain of the urban-rural divide.
Throughout high school, I suffered from headaches. Every few months I would visit a local neurologist. Senior year, the headaches worsened and after a visit to the neurologist, I had another MRI. My family called into the office to ask if there had been any change demonstrated in my scan. They answered that no change was evident on the scan. As a result, my family and I assumed that there was nothing further that needed to happen with my care. I continued with my everyday life.
However, in the first few months of college it became clear that something wasn’t right. I had begun to lose feeling in my extremities, I was throwing up every day, and my pain had become unmanageable. I was sent for another MRI scan, this time at Duke Hospital. When receiving the MRI contrast, I felt as if I was boiling hot and had difficulty breathing. Quickly, epinephrine was administered, I was whisked away, and stayed in the hospital overnight. The staff around me bustled nervously and I caught snatches of whispered conversations, “… contact neurosurgery…” “… how soon can she get an appointment?” A few days after leaving the hospital, Duke Pediatric Neurosurgery contacted me to schedule an appointment, they offered one within the week. I was shocked. When I had separately attempted to get an appointment with Duke neurology, they had suggested a date six months away.
At my appointment, the neurosurgeon spoke softly to me, informing me that he now considered himself a part of my family as he showed me images of my brain. I still didn’t understand. Then, what he had been leading up to: he recommended brain surgery within the next month. There had been significant unaddressed change regarding pressure in my brain and my spinal fluid flow was dangerously blocked. A sickening feeling crept over me, a lump formed in my throat: I had slipped through the cracks of the broken rural health infrastructure. It had all been up to chance. I was forced to confront my situation head on as I faced the possibility of losing a large portion of my hair, navigating the healthcare system, dealing with numerous side effects, and still managing academic responsibilities.
Everyone, regardless of region, income, or anything else, has the right to adequate and responsible health care.
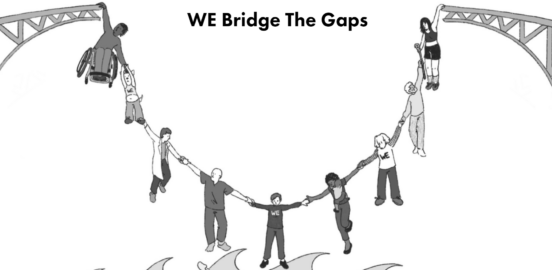
I envision a world in which no one’s health is left up to chance. I refuse to accept that ‘sometimes people just fall through the cracks.’ Everyone– regardless of region, income or anything else– has the right to adequate and responsible health care. My story does not stand alone. It is one of many, as millions of Americans grapple with the reality of a health care system that has left rural communities behind. Not only is there a severe deficit of health care providers in rural areas, oftentimes forcing residents to travel hours for care, the health care provided can be gravely outdated. With a system not built to save, the opposite occurs, and the tragic truth is that many people do ‘slip through the cracks.’ The time has come when we as a country can no longer stand by as lives are lost. Change is not an option, it is a necessity.
In the aftermath of brain surgery, as my body healed and I no longer appeared ‘sick,’ I never forgot the way I felt. I realized that raising my voice, no matter how daunting and raw it might be, has the ability to amplify the very real problems faced by the community I care so deeply about. My own story, and that of those around me, has left me driven to learn more every day and to advocate for change. This is why I am so passionate about patient advocacy. Patient advocacy is bringing to light the challenges faced by many. Patient advocacy is amplifying patient stories to bring about informed solutions. Patient advocacy provides hope for a future where access to care and to legal resources is within reach for all.
Caregiving, Health Literacy, Needs Navigation, Trust
Equity, Policy Consortium
Equity, Palliative Care
Equity, Health Literacy, Insurance, Policy Consortium



